For The Weekly Pulse (a revisit of an old Ms. column!), we’ve scoured the most trusted journalistic sources—and, of course, our Twitter feeds—to bring you this week’s most important news stories related to health and wellness.

In this edition: We are back with continued coverage of the coronavirus pandemic, including updates on vaccine distribution; a look at hospitals that are overflowing yet understaffed; and Argentina’s legalization of abortion as the highlight of this week’s repro rundown.
Pandemic Updates
+ Though the advent of a vaccine has offered hope, the U.S. is currently experiencing the worst phase of the pandemic thus far. Fueled by holiday travel and gatherings, the current surge has led to a rate of one American dying from COVID-19 every 33 seconds. According to the Johns Hopkins Coronavirus Resource Center, more than 3,800 people lost their lives due to COVID-19 on Wednesday—a record high for daily deaths in the U.S.
Even so, Dr. Fauci and other health experts agree we haven’t yet witnessed the full fallout of the post-holiday surge. More than 360,000 people have already died due to the pandemic in the U.S.
+ Shortly after scientists identified a new, more contagious strain of the coronavirus in England, the first cases of infection from the new strain were identified in the U.S. and in other countries. While there is no evidence at this time showing the new strain to be more deadly or causing a more severe course of disease, it’s still concerning to public health officials because it could add even more stress to the already-struggling health care system.
Luckily, scientists predict that the COVID-19 vaccines will still work against the new strain—vaccines tell our bodies to create antibodies against the virus, and these antibodies will still recognize the virus even when small mutations occur.
+ While The Weekly Pulse was on break over the holidays, Congress passed a $900 billion coronavirus relief package. Importantly, the deal provides direct aid to struggling Americans through a $600 dollar stimulus check for those making under $75,000 per year, and extends federal unemployment benefits for another 11 weeks. The bill also includes $69 billion in funding for vaccine distribution and other public health measures.
Many, including President Trump himself, criticized Senate Majority Leader Mitch McConnell (R-Ky.) for blocking $2,000 stimulus checks. However, the $2,000 stimulus payments could still become a reality. The Democratic victories in both of Georgia’s Senate run-off elections this week paves the way for the Biden administration to work with Congress to pass another stimulus bill soon after the new president takes office.

Vaccine Rollout Faces Hurdles
+ Rolling out the COVID-19 vaccine to millions of Americans was never going to be an easy task, but it’s still been frustratingly slow. In a recent interview, Dr. Fauci pointed to the holiday season as one reason for the slow rollout. Additionally, the lack of federal requirements on vaccine distribution is causing tension as individual states and hospitals are left alone to decide who to vaccinate first. Along with shipping delays, the many challenges of distribution has meant that only only 2.8 million doses of the vaccine were administered by the end of 2020, despite the federal government’s initial goal to vaccinate 20 million people before the new year.
+ The haphazard rollout has left the public confused about when, where and how to get the vaccine. Without a nationwide plan, getting a vaccine can vary widely from county to county and state to state. Glitchy appointment websites, tightened state restrictions on vaccine prioritization and logistical issues are leaving precious vaccine doses to expire.
Governors are being WAY too precious about who gets this vaccine and we’re going to end up with millions of doses of expired vaccines if states don’t get serious about getting this out the door. These numbers are dangerously bad https://t.co/9VBv9nSEkr pic.twitter.com/RciNui1kSn
— Ryan Grim (@ryangrim) December 30, 2020
Experts are still optimistic that the U.S. can improve vaccine distribution in the coming weeks by streamlining the process. For example, New York City is investing in pop-up vaccination sites, along with “vaccination hubs” that are set to remain open 24 hours a day. The Biden administration has criticized the Trump’s administration’s hands-off approach in the distribution process. President-Elect Biden set a goal of administering 100 million shots in his administration’s first 100 days.
“I’m going to move heaven and Earth to get us going in the right direction. I’m going to use my power under the Defense Production Act, when I’m sworn in, in order—and order private industry to accelerate the making of the materials needed for the vaccines as well as protective gear,” Biden said.

+ Early reports of allergic reactions to the vaccine fueled doubt about the vaccine; however, there have only been 21 incidents of people experiencing a severe allergic reaction out of more than 2 million vaccinations. According to the CDC, these incidents are both rare and treatable, meaning the danger of a COVID-19 infection far outweighs the risk of vaccination.
Furthermore, both the FDA and the NIH are investigating the cause behind these incidents. As an extra precaution, the CDC recommends people who receive the vaccine are monitored for at least 15 minutes afterwards, or 30 minutes for those with a history of allergic reactions to vaccines.
Hospitals Understaffed and Overflowing
+ As cases of COVID-19 surge, hospitals in at least 25 states have reported extreme shortages of nurses, doctors and other critical staff. Even with stockpiles of protective gear and medical equipment, these supplies are of little to no use without a stable staff. In some cases, severely ill patients have even been transported hundred of miles for care.
“Care is about more than a room with a hospital bed. It’s about medical professionals taking care of patients,” said John Henderson, chief executive of the Texas Organization of Rural & Community Hospitals (TORCH). “If you don’t have the staff to do that, people are going to die.”
+ The state of California has ordered hospitals with the room to accept more patients to begin accepting transfers from hospitals who have run out of beds.
“If we continue to see an alarming increase of COVID-19 patient admissions at hospitals statewide, some facilities may not be able to provide the critical and necessary care Californians need, whether those patients have COVID-19 or another medical condition,” said Dr. Tomas J. Aragon, the state’s public health officer.
Following the latest surge in COVID-19 cases, officials were citing a shortage of beds and staff as the virus threatened health care systems. In Los Angeles, health officials ordered first responders to stop bring adult patients who are unable to be resuscitated to hospitals for care.
“Patients in traumatic full arrest who meet current Ref 814 criteria for determination of death shall not be resuscitated and shall be determined dead on scene and not transported,” said Marianne Gausche-Hill, medical director of the Los Angeles County Emergency Medical Services Agency.
+ In California, some ambulances carrying patients are having to wait as long as eight hours before meeting with hospital staff—delays which could cost lives. Ambulances are also being advised to cut back on their use of oxygen and only administer it to patients with oxygen saturation levels below 90 percent.
“Many hospitals have reached a point of crisis and are having to make very tough decisions about patient care,” said Dr. Christina Ghaly, the L.A. County director of health services.
+ The Alabama health care system—with the nation’s third highest number of people per capita hospitalized with the virus—is close to reaching a breaking point. Nearly half of the patients being treated at the Northeast Alabama Regional Medical center are being treated for symptoms or complications related to COVID-19, and the hospital is cutting any services it can in order to free up staff and space.
“We’ve closed our orthopedic unit and turned it into a COVID unit,” said CEO Louis Bass. “We closed our Peds GYN unit and made it COVID. Our most recent thing is where we closed our primary medical unit.”
Bracing for yet another surge and coping with the current rise in cases, hospitals will soon have to stop accepting transfer patients.
+ In Arizona, local hospitals overwhelmed with COVID care asked for ambulances to be directed to other facilities do to a lack of capacity. Statewide, 62 percent of ICU patients have COVID-19 and only 8 percent of ICU beds are available.
As of January 1, Banner Health, Arizona’s largest hospital chain, made the decision to halt any and all elective surgeries in order to conserve medical staff, supplies and space.
+ Around 20 percent of the 240 hospitals a part of the Ohio Hospital Association have reported staffing shortages, says spokesperson John Palmer.
+ ICU nurses who typically care for no more than two patients at a time are now being asked to care for as many as six to eight patients at a time due to a lack of staff, reports Robert Hancock, president of the Texas College of Emergency Physicians.
+ As Missouri continues to become overrun with COVID-19 cases, the state has hired Vizient, a health care performance improvement company, to provide hospitals with temporary workers and additional beds. The state says their 12-week partnership will run though February and could be extended depending on the state of the pandemic.
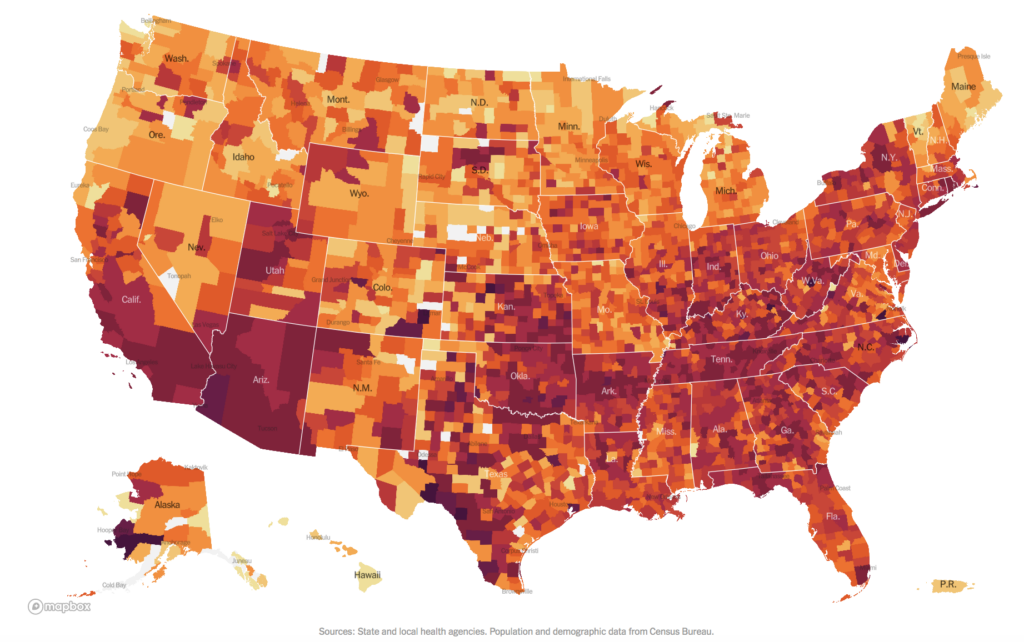
+ To allow individuals the opportunity to check-in on their local hospital capacities, NPR has released a tool to track which hospitals are dangerously full this week. The interactive map follows the federal government’s release of an updated set of detailed hospital-level data to show how many inpatient and ICU beds are available weekly.
Repro Rundown: Victory in Argentina!
+ On December 23, Argentina became the largest Latin American nation to legalize abortion. This historic victory for reproductive rights came following a tireless grass-roots movement, rallying cries heard around the world and a landmark vote within the extremely conservative region.
The Argentine Congress voted 38-29 (with one abstention) in favor of legalizing abortion care up to the 14th week of pregnancy—a larger margin than anticipated.
Senator Silvina García Larraburu—who voted against the bill in 2018 but backed it in 2020—said during the debate: “My vote is in favor of free women, of women who can decide according to their own conscience.”
+ Both chambers of the Massachusetts state Congress joined together to pass The ROE Act, legislation that not only solidifies, but expands abortion health and rights in state law by overriding Gov. Charlie Baker’s recent veto of the measure.
“Pregnant people who once faced near-insurmountable barriers accessing abortion care can now seize the right to control their own bodies,” Sen. Harriette Chandler said in a tweet Tuesday.
“With the ROE Act provisions now law, most young adults seeking abortion will be able to access the care and support they need without navigating the court system, and pregnant people facing a fatal fetal diagnosis later in pregnancy will be able to access abortion care here in Massachusetts, with a provider they know and trust, rather than traveling across the country for care,” organizers said in a statement.
+ According to a new study published in the Journal of the American Medical Association, the number of Texas residents who sought to receive out-of-state abortion care jumped from 157 in February to 947 in April. This increase is linked to Gov. Greg Abbott’s order to halt any and all procedures not “immediately, medically necessary” in the wake of the COVID-19 pandemic.
+ Just as the year was coming to a close, Ohio Gov. Mike DeWine signed a bill requiring any aborted tissue to be buried or cremated following the procedure. The bill also places the responsibility of that decision onto either the patient or the clinic, penalizing whoever fails to make the decision.
Any and all financial responsibility falls upon the patient.
“This is honestly just a familiar ploy by these lawmakers who use the chaos of the end of year session to try and pass these unpopular bills,” Laurel Powell of Planned Parenthood Advocates of Ohio said. “Studies have repeatedly shown that the majority of Ohioans support access to safe and legal abortion care.”
+ A new study published in Human Reproduction reports that a sperm-producing partner’s poor health before conception may increase the risk of pregnancy loss.
The study analyzed data from 958,804 pregnancies between 2007 and 2016 through an employee insurance database, as well as information on the parent’s health averaging about four years before conception. Researchers scored the sperm-producing parent’s health based on five pieces of the metabolic system which includes: diagnosis of hypertension, high cholesterol, obesity or diabetes, as well as the presence of other common chronic illnesses.
Compared to sperm-producing partners who presented none of the five areas of poor health, those with one had a 10 percent increased risk of “siring a pregnancy that ended in loss,” those with two had a 15 percent increased risk and those with three or more increased that risk by 19 percent.
You may also like:





