“We now have an exciting opportunity to create a new abortion system that is more equitable, accessible and affordable in all 50 states,” Dr. Angel Foster, medical director of the Massachusetts Medication Abortion Access Project.

Close to two-thirds of all abortions obtained through the formal medical system are now done with abortion pills. Almost one-fifth of abortions are done through telehealth consultations with clinicians, who then abortion mail pills to eligible patients. Since Dobbs, an increasing number of abortion providers are providing telemedicine abortion services to women living in states banning abortion.
Eight states have passed laws allowing clinicians to provide telehealth abortion care to out-of-state patients and shielding them from criminal and civil liability in anti-abortion states. In the second half of 2023 alone, over 40,000 women in states with severe abortion bans or telehealth restrictions received medication abortion from healthcare providers located in states with provider shield laws, including Massachusetts, Washington, Colorado, Vermont, New York, California, Maine and Rhode Island.
Today there are four practices with over two dozen providers that provide telehealth abortion services to people in restrictive states. One of them is the Massachusetts Medication Abortion Access Project, called The MAP for short.
The MAP provides telemedicine services to people aged 16 and over who are up to 11 weeks pregnant in all 50 states for a sliding scale fee of up to $250, with two- to five-day delivery of abortion pills. The MAP has four clinicians all licensed and residing in Massachusetts, who have served over 3,500 patients since they began offering telehealth abortion in October 2023.
Ms. spoke with the medical director of The MAP, Dr. Angel Foster, who is a Harvard-trained obstetrician/gynecologist and health sciences professor at the University of Ottawa, where she leads a large research group that’s dedicated to global abortion work.
This interview has been lightly edited for clarity.
Carrie N. Baker: Why did you start The MAP?
Dr. Angel Foster: Our first goal is to provide high-quality, safe, affordable abortion care to patients who are residing in banned or restricted states. Our second goal is to demonstrate the strength of the shield law. Our third is to create a model that could be tailored and replicated in other states.
Baker: How did you start it?
Foster: When Massachusetts passed its shield law in July of 2022, a small group of us started developing a shield law practice. After medical school, I participated in the first rigorous research on the safety and efficacy of misoprostol alone for abortion through de-medicalized strategies of service delivery in Thailand, Pakistan, Jordan, Uganda and other settings. A lot of what we learned from our de-medicalized medication abortion work in the global south informed the way that we approach The MAP and our comfort level with providing this care in the wake of Dobbs.
Baker: How does your service work?
Foster: Patients find out about our service through a consolidator website, such as Plan C or I Need An Abortion. On our website, we provide a lot of information about how our service works. The prospective patients fill out a brief eligibility screening form with some basic questions, including contact information, age, date of birth and last menstrual period, as well as the state, territory or APO address that the pills will be sent to. We serve patients who are within 11 weeks from the first day of their last menstrual period. Most of our patients contact us before seven weeks.
Once the basic screening form is filled out, one of our team reviews it, makes sure they’re eligible and then sends a link to a medical questionnaire and consent forms for the patient to sign. The questionnaire takes somewhere between five and 10 minutes to fill out, depending on how complicated the person’s medical history is. We ask basic medical history that’s relevant to providing care. A clinician then reviews the questionnaire and approves the patient. The patient will then receive an email asking them to pay.
Baker: How long does the eligibility process take?
Foster: In general, it’s a couple of hours. We have people who are operating our systems from about 6 a.m. until 11 p.m.. We try to turn requests around quickly. We’ve had patients who have gone from filling out the initial form to paying within an hour. We try to get back to patients in all cases within eight hours, and I would say, in most cases, it’s within four.
Baker: What do you charge, how can people pay and do you take insurance?
Foster: We do not take insurance. Our service costs $250, but we use a pay-as-much-as-you-can model, no questions asked. We trust our patients. We do ask that patients make a five-dollar minimum payment, which we waive on a case-by-case basis.
They can pay through PayPal, Cash App or Zelle. Once a patient pays, we send the pills via USPS Priority Mail. We usually mail the pills either the same or the next business day after we’ve received the payment, and USPS Priority Mail takes 2 to 5 business days. If they pay the full amount and an additional 25 dollars, we will use Express Mail so they can get the pills the next day.
Baker: How are you able to offer the sliding-scale fee?
Foster: We had some initial foundation grants that helped us get started. We now work with about a dozen abortion funds, both national and local. Also, we’ve got individual donations that come in as well.
A third of our patients pay 5 dollars or less, a third of our patients receive a subsidy of some kind and a third of our patients pay 250 dollars. We’re able to do this because a lot of us are doing this as either volunteers or at below-market rates. Two of our clinicians volunteer their time. One of them volunteers part of her time. We pay a living wage to our office staff.
Our model is going to change on October 1. All of the core costs of the service will be covered by foundation grants and we will provide care for 5 dollars or more, rather than 250 dollars or less. We’re hoping that we’ll be able to secure patient payments of the 60 dollars that it costs us to cover the meds, the postage and the package. I’m excited about this experiment. It’s a first step in trying to pilot a very different model of care.
Baker: This seems like a much more affordable way to provide abortion healthcare than funding people to travel long distances for in-clinic medication abortion.
Foster: It is. We can provide about 15,000 abortions next year under this model based on our current setup. It ends up costing us about $33 per abortion compared to the average cost of an in-clinic medication abortion of about $600 plus travel.
Baker: What medications do you send to patients?
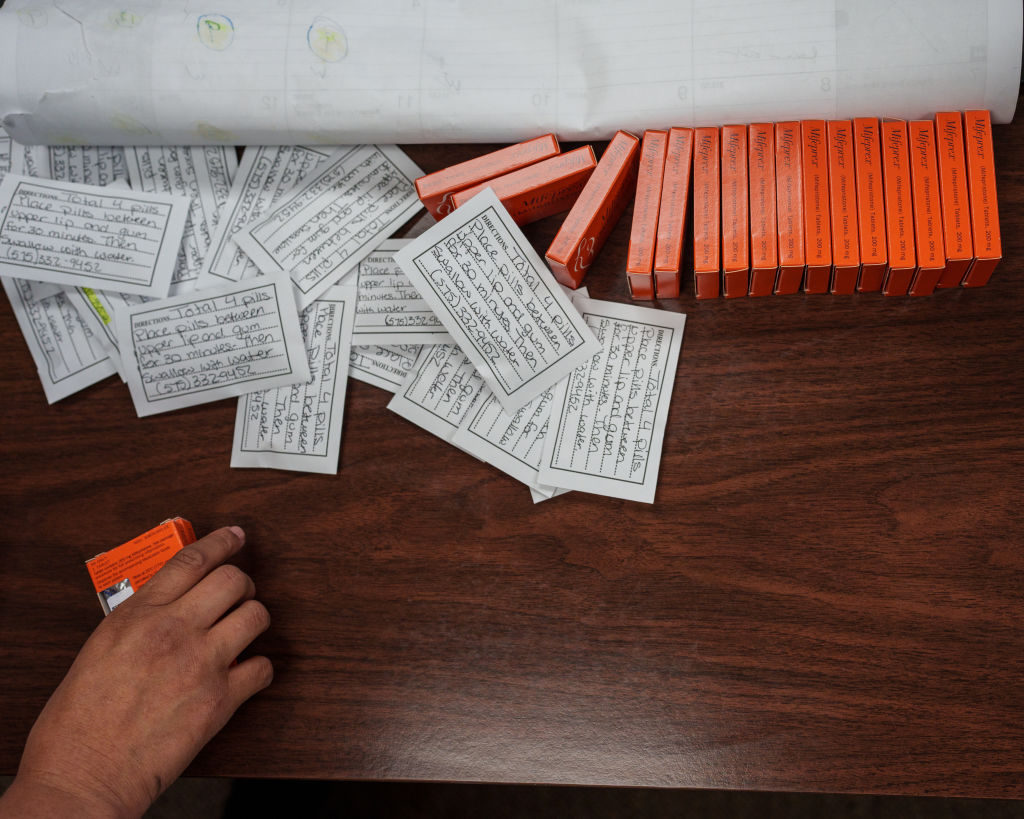
Foster: We send one mifepristone pill and eight misoprostol pills for anyone under nine weeks of pregnancy, and one mife and 12 miso for anyone who’s nine weeks and above. In comparison to in-clinic care, we give an extra dose of miso gestationally. The reason that we ask them to take additional pills is to get the effectiveness up so that they don’t have to follow up in person because we want to avoid having them go to in-person follow-ups if we can help it.
Baker: Does taking an extra four Miso make it harder on patients?
Foster: You’re going to have a little bit more cramping and transient diarrhea, but we feel like that extra miso is beneficial because it can get us higher completion rates. We think it’s worth that tradeoff, and we encourage everyone to take all the drugs we give them.
Nine-five percent of our patients are from states that restrict abortion or telemedicine abortion.
Dr. Angel Foster
Baker: What guidance do you give your patients about how to use the medications?
Foster: We instruct them to take the misoprostol 24 to 48 hours after they’ve taken the mifepristone. We encourage everyone to take misoprostol buccally (in the cheek pouch) and swallow the pill remnants so there’s no residue in case they need to go to an emergency department. In our materials, we give them language that they can use if they go to an emergency department and don’t want to disclose that they’ve taken abortion pills.
We provide pills for immediate use, but we also provide pills in advance of need, and we provide period pills so they can be used around the time of an expected period, but before a positive pregnancy test. We provide information about how to take the pills in these different scenarios. We also provide information about how to use mifepristone as emergency contraception if a patient wants to do that, particularly for pills that have been procured in advance of need. Mifepristone in hand works as well if not better than Plan B and progestin-only emergency contraception.
Baker: What other resources do you give to patients when you send the pills?
Foster: When the patients receive pills from us, they get information about ectopic pregnancy precautions. We tell patients how to contact Bedsider if they want to talk about contraception options, Repro Legal Helpline if they have legal questions and the Miscarriage and Abortion Hotline if they have any medical questions. Then we provide them with information about reproductive health clinics near them in case they want to see a provider that is pro-choice. That’s not available in all states. We also provide a digital privacy protection card about how to keep their information private, both in terms of what they should do with the physical materials we’ve sent, but also how to delete their online footprint. Finally, we provide them with a little handwritten card.
Baker: What follow-up care do you provide to your patients?
Foster: All of our patients get a phone number for our service that we only provide to patients. We’re available 6 a.m. to 11 p.m. We get back to people quickly. We also have a secure email, and we use text. We send a questionnaire to our patients two weeks after we send the pills and then six weeks after.
Baker: Are your patients satisfied with your service?
Foster: They love it. We get such great feedback. We’ve had a very small number of adverse outcomes in terms of continuing pregnancies or people needing to visit an emergency department for medical reasons.
Baker: How many patients have you served since you opened in October of 2023?
Foster: We have served around 3,500 patients overall so far. We’re serving about 500 patients a month now.
Baker: What’s your success rate as far as completed abortions?
Foster: We are in the 98 percent range—outcomes very comparable to in-clinic care.
Baker: Of those 3,500 patients, are they all coming from the states that ban abortion or restrict telemedicine?
Foster: Nine-five percent of our patients are from states that restrict abortion or telemedicine abortion. About a third of our patients are from Texas. About a third of our patients are from Florida and Georgia, with a smattering of other states, including Alabama and Louisiana. We serve a small number of folks who are in high-access states.
Baker: Do you require patients to provide identification?
Foster: We do not.
It’s been really exciting to see the amount of community support. The more ownership that people feel of this, the more protected we are. That’s a really important part of distributing risk as well.
Dr. Angel Foster
Baker: What kinds of precautions do you take to protect the individuals involved in your organization from being targeted?
Foster: The whole project is set up around distributed risk. Different people order our pills, package our pills, process the money, write the prescriptions and take the pills to the post office, which makes it harder to identify individuals as opposed to the practice.
In general, there’s a commitment that people aren’t going to travel to or through banned states, especially states like Texas and Idaho, where it appears that there are attorneys general or others who would like to make a case against shield law providers.
How our individuals choose to protect their assets in order to potentially withstand any kind of civil suits or decisions about travel are based on individual risk tolerance. Not all of the people who work with The MAP are public-facing.
We trust members of our team to make the decisions that are right for themselves, given their personal stories, lives and relationships. We also trust that the Commonwealth has our back and will protect us if folks come after us.
Baker: Has the community in Cambridge supported you?
Foster: There’s been a lot of support in Massachusetts. We have a huge group of volunteers who work with our service. Twice a month, we have pizza and packing parties, where people come to our office and pack up the boxes for mailing. We’ve got somebody with clinic management experience who’s volunteered to manage some of our data storage issues. We have people who are working with us to develop newsletters. It’s been really exciting to see the amount of community support. The more ownership that people feel of this, the more protected we are. That’s a really important part of distributing risk as well.
Baker: Is the Massachusetts telemedicine abortion shield law as strong as you’d like it to be, or are there improvements that the state could make?
Foster: The Massachusetts shield law is the most comprehensive in the country. It protects clinicians, helpers and funders from criminal, civil and licensure penalties. We would love to see more work on how to strengthen interstate shield protections and reciprocity, but that has to be done in conjunction with the other states.
Baker: What about physical security at your office?
Foster: We chose an office space that’s over a large cannabis dispensary because they are quite well-regulated and have security features and cameras. We also chose a space that was hard to protest. We’re in a very busy pedestrian area in Davis Square.
Baker: Do you have any final thoughts?
Foster: There’s a deep irony post-Dobbs. Things have been absolutely terrible for obstetrics, but it hasn’t been nearly so bad for medication abortion. The reality is in states like Missouri, Texas or Mississippi, medication abortion is more available and affordable now than it was before Dobbs. Now we have this opportunity to provide care to folks throughout the country in a way that we haven’t had before. We now have an exciting opportunity to create a new abortion system that is more equitable, accessible and affordable in all 50 states.
Baker: How can Ms. readers support your work?
Foster: We accept individual donations, large and small. The other way that Ms. readers can help is to let people know that high-quality, safe, FDA-approved abortion medication is available to people in all 50 states, and that shield laws allow this. One of the challenges that we face is a legitimacy challenge. People trust sources that are close to them, that are known to them, that are within their families and communities, so spreading this message locally is really important.
To donate to The MAP, go here.
Read more:
U.S. democracy is at a dangerous inflection point—from the demise of abortion rights, to a lack of pay equity and parental leave, to skyrocketing maternal mortality, and attacks on trans health. Left unchecked, these crises will lead to wider gaps in political participation and representation. For 50 years, Ms. has been forging feminist journalism—reporting, rebelling and truth-telling from the front-lines, championing the Equal Rights Amendment, and centering the stories of those most impacted. With all that’s at stake for equality, we are redoubling our commitment for the next 50 years. In turn, we need your help, Support Ms. today with a donation—any amount that is meaningful to you. For as little as $5 each month, you’ll receive the print magazine along with our e-newsletters, action alerts, and invitations to Ms. Studios events and podcasts. We are grateful for your loyalty and ferocity.





