As we await the fate of Roe v. Wade, Ms.’s “Online Abortion Provider” series will spotlight the wide range of new telemedicine abortion providers springing up across the country in response to the recent removal of longstanding FDA restrictions on the abortion pill mifepristone.
“Patients, a lot of them, don’t need a lot of counseling. A lot of people just know they want an abortion.”
—Dr. Jamie Phifer, founder and medical director of Abortion On Demand
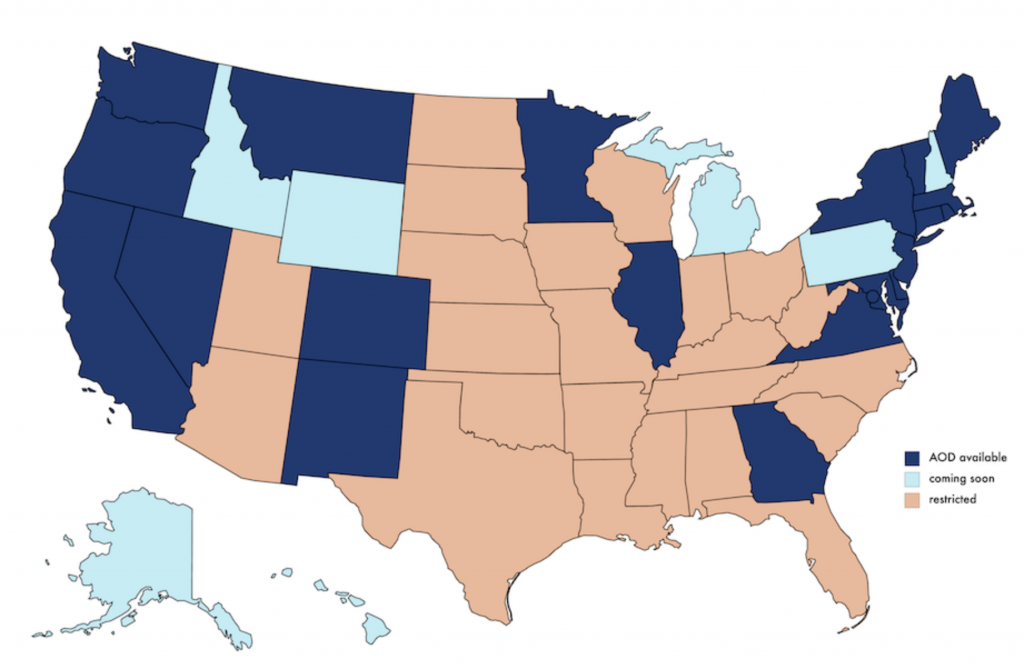
Abortion On Demand (AOD) is a new telemedicine abortion startup that uses innovative technology to provide abortion pills to patients by mail in early pregnancy at an affordable price ($239 versus the national average of around $500). Offering services in 20 states and Washington D.C., AOD is the first large-scale telemedicine abortion provider run by a U.S.-based doctor.
The founder and medical director, Dr. Jamie Phifer, has over a decade of experience providing medically complex abortion care at independent clinics. When the FDA recently lifted restrictions on mailing abortion pills during the pandemic, Phifer realized her dream of making medication abortion easily available to patients by telemedicine and mail. Using secure platforms that meet federal and state privacy standards, AOD serves people 18 years old and over, who are pregnant up to eight weeks at intake.
But Phifer was concerned about the economic impact of telemedicine abortion startups on independent, brick-and-mortar clinics. To ensure they stay in business—and that pregnant people will always have a place to go when they need or want in-clinic care—AOD donates a majority of their profits to Keep Our Clinics, supporting independent abortion clinics.
Ms. sat down with Dr. Phifer to learn more about Abortion on Demand and the future of telemedicine abortion.
Carrie Baker: When did you launch Abortion on Demand?
Jamie Phifer: On April 16. I’m very happy to now be seeing patients. We are up and running in 20 states. It’s been an interesting first month for sure!
Baker: How many people have you seen in your first month?
Phifer: We’ve seen 80 patients in four weeks. We should eventually be able to scale up to 20,000 patients in a year because of the automation.
Baker: I noticed on your site you say people can get same-day appointments and then have the medications mailed overnight. How does that work?
Phifer: It’s called Abortion On Demand for a reason. The schedule is set up on a rolling basis based on how many patients begin scheduling throughout the day. Almost everyone is scheduling either the same day or the night before. Patients do a video consult usually same day or the next day and then we use express overnight shipping for everybody. There’s no extra payment for express shipping or for the comfort medications. Everyone gets the exact same treatment and pays the same amount—$239.
Baker: Do you take insurance?
Phifer: No.
Baker: Can you explain the process for getting an appointment through the website?
Phifer: Patients go through intake by filling out an online form. Then once they’re done with the intake process, it automatically routes them to scheduling for appointments. In the later part of the day, it might be difficult to get in the same day, but patients certainly should have appointments available the next morning. All they do is select an appointment time, and they get a confirmation email that has a link to our virtual waiting room. They get a text reminder about 20 minutes beforehand whenever their appointment is. People don’t have to schedule same day. The scheduling is open for up to seven days out.
Baker: What happens at the appointment?
Phifer: Using the link we send them, they check-in and enter the virtual waiting room. Eventually, we’re going to have a counseling video in the virtual waiting room that goes over everything and they’ll have a link to that video so they can go back and review it any time. We’ll also have information that’s written in digital form and on paper that we’ll send to them.
Then they do the real-time video with the physician, who will review the key points, address some of the issues that are required to be addressed by the FDA, and make sure that the patient understands all of that. The doctor then sends the paperwork to the patient, which depending on the patient could take five minutes or 20 minutes. We use a secure digital platform to send the informed consent form. Most patients don’t seem to have many questions. Everyone gets the exact same process except for our two states that have a 24-hour waiting period—Georgia and Minnesota. We accommodate that by setting a timer between when we receive the digitally-signed Informed consent documents and when the order gets shipped to the pharmacy partner.
Baker: How have the video conferences been going so far?
Phifer: Most people when I get on video with them, they are just excited. Their first thing is, “I didn’t know I could do this!” And you know, the people would be either in their bedrooms or sitting in their car on their lunch break. I have a lot of patients who are already parents and they’re hiding from their kids who are doing virtual school. They do the visit on their phones in their car. They didn’t have to arrange child care, they didn’t have to take any time off work, it just shows up at their doorstep.
Baker: Which online pharmacy do you use?
Phifer: American Mail Order Pharmacy. It’s shipped overnight right around 5 or 6 p.m. Eastern time. Patients should get a confirmation email with their tracking number in the evening if they’re on the East Coast, late afternoon on the West Coast. Everyone in an urban area, at least so far, has gotten their medications by the end of that next day.

Baker: If they have any questions, are you available by phone or by text?
Phifer: Yes. There’s a 24-hour phone line that has a physician on-call 24/7. I’m the primary physician so it’s almost always me. And then we have an administrative phone line that routes to a voicemail for non-urgent issues. Both of those phone numbers can accept text messages if the patient is comfortable with that. But we ask patients to call the urgent line at first rather than text to ensure urgent medical issues are addressed right away.
Baker: Are you getting many calls after patients take the medications?
Phifer: The amount of follow-up calls seems to be relatively low. I think there are probably some factors that go into that. One is patients are comfortable. They’re in their own homes so the anxiety is a little bit less. When they’re getting their counseling or talking to the physician, they’re in a space where they didn’t have to navigate past a line of protestors. They’re in their own space and they can comfortably ask the questions they need to ask. I feel like I’m getting fewer urgent calls about questions that I know I’ve already addressed because I feel like patients are much more engaged because they’re less anxious.
We’re also seeing people so much earlier in their pregnancies—roughly between four and six weeks seems to be the most typical. The phone calls I’m getting—instead of people worried about heavy bleeding—they’re worried that they’re not bleeding enough and they assume it didn’t work. But what’s happening is I’m citing data from what the average amount of the bleeding should be for in-person care, but in-person care is often delayed by one to two weeks depending on when they schedule. I think we’re going to have to change our counseling to say don’t be surprised if you only have a medium amount of bleeding, it’s probably because you got care so early.
Baker: What about follow up after the abortion?
Phifer: It’s automated follow-up by text four days after their appointment. The text says: Hi from AOD, we expect you took both medicines by now. If so, click here to answer some survey questions—and there’s a secure survey link that’s tied directly to their cell phone number where they click on it. They tell us what day they took the medications, and then whether they had the expected amount of bleeding. And if they answer the question in a way that’s at all worrisome—a signal that we should check in—then it routes automatically to the call center. For the person answering that phone, they know that specific call is about making sure that they did in fact have the bleeding that was expected.
And then the other automated follow-up is in 16 days to ask them to take a pregnancy test. We send a low-sensitivity pregnancy test to everyone, what I would call a medical-grade pregnancy test. It turns negative much sooner than the over-the-counter tests. We give instructions for folks on how to do it and that’s included in the text-based follow-up. We coach patients during their video visits not to try to take the pregnancy test early because it’ll still be positive. We give them the medical-grade test as an extra reassurance because then they’ll know that the test turned negative within two weeks instead of waiting a full four weeks for the over-the-counter ones to turn negative.
Baker: Has everybody had a successful experience so far?
Phifer: So far. I have not had a single “failed” medication abortion. The failure rate is less than two percent so it may just be that we haven’t had enough patients.
Baker: Any complications so far?
Phifer: No. The actual complication rate of medication abortion is so extremely low. The most common “risk” is that it might not work. That someone might be in the one and a half percent of women for whom it doesn’t work. But because we’re doing those really close follow-ups, we should in theory be able to catch that really quickly.
Baker: How late in a pregnancy can someone make an appointment?
Phifer: Fifty-six days gestation for the intake, not necessarily for their appointment. They can say that they had their last menstrual period eight weeks ago exactly and then schedule their appointment another week out, that’s fine.

Baker: Why did you start Abortion on Demand?
Phifer: I had been talking with colleagues about telemedicine medication abortion for years. The enforcement of the REMS [Risk and Evaluation Mitigation System] has always been the barrier but that has been suspended for now. Also, during the pandemic, more patients were comfortable with telemedicine, so that was an opportunity for people to be comfortable with telemedicine abortion.
Abortion care is easy. Medically speaking, it is easy enough that a robot could do it. So we built the robot and it is trying to mimic the closest thing to over-the-counter medication where there’s essentially a checklist. Down the line hopefully the FDA will not enforce the REMS. Our model is dependent on the REMS not being enforced.
“Abortion care is easy. Medically speaking, it is easy enough that a robot could do it. So we built the robot.“
Baker: Tell me about why you donate the majority of your profits to independent clinics.
Phifer: I’m concerned about the impacts telemedicine abortion may have on brick-and-mortar clinics. Our costs of providing care are lower. We’re not paying insurance on a building. We don’t have a facility per se. We don’t have many staff. Those two big costs that brick-and-mortar practices have to keep up, we don’t have, we can provide care at a lower cost. They also have to hire security against protesters.
I’m concerned that because of the low cost of providing telemedicine, someone will eventually do this abortion care at scale thinking that they’re being really helpful but not actually considering these brick-and-mortar clinics and the impact that it will have on them. I’m worried that very well-meaning startups, small businesses, even pre-existing telehealth providers will say “oh, look, abortion is medically uncomplicated, it should be easy to provide access to people using our infrastructure.”
But if the patients who would just use telemedicine abortion are not going to brick-and-mortar practices, there’s a risk that the brick-and-mortar practices might close. Then where are patients going to go? Anybody who’s over 11 weeks, who is medically complicated, or frankly just wants a procedure, or even just wants to see a doctor in person for their medications? I’m worried about those who are less likely to speak English, less likely to have reliable income, less likely to have a reliable residential address, less likely to have a smartphone with a video camera. If clinics that have been providing access for that patient population for 50 years now can’t keep their doors open, where will people go? Many people who would use telemedicine abortion, they’re going to get access no matter what. They’re not the folks I’m worried about. It’s everybody else.
I launched AOD at scale in these 20 states all at once so that the per patient cost is relatively low for AOD, which means that our margins are wider and we can donate the IRS maximum back to in-person clinics. We give 60 percent of our profits to Keep Our Clinics of the Abortion Care Network—the professional group for independent abortion clinics. The indie clinics is where my heart is. I originally trained to do late gestation care there. They stick their necks out for patients. Yet they’re the most vulnerable to fewer patients coming in and less funding. Whenever there’s an issue around abortion access nationwide, everybody throws their hands in the air and donates to Planned Parenthood. But in a lot of states, it’s just indie clinics. And the indie clinics are the ones bringing the court cases. Folks who have access and will always have access are essentially offsetting the costs of taking their care out of the brick-and-mortar practices.
Baker: Have you heard of any clinics being negatively impacted by telemedicine start ups?
Phifer: I just got off the phone with a brick-and-mortar practice that was forced to triple their marketing budget to stay afloat due to aggressive marketing by a telehealth start up in their state. I’m getting very worried online mifepristone start-ups will force closure of the only sites available to vulnerable and late gestation patients. I’m hoping AOD’s donations can help clinics like theirs survive this rapid change.
Baker: Why did you name your start up Abortion on Demand?
Phifer: It’s called Abortion On Demand for a reason. It’s provocative, I know. But when you’ve already decided that you don’t want to continue your pregnancy, especially if you have pregnancy symptoms, making people wait doesn’t feel right to me. The standard should not be that people have to go to an in-person clinic or even to wait for your pre-scheduled visit with a telehealth provider, or wait five days for your medications to show up.
For my own professional curiosity, I also wanted to prove that you could get people care safely and this quickly. I hope that it will be the norm down the road. I think one of the ways to help ensure that it is the norm is to launch it at scale—to see a bunch of patients and get a lot of data from those patients. It’s one thing to be operating in one state and trying it out. It’s a totally different thing to say we’re going to see up to 10 percent of the medication abortions in all of these states—that would be over 20 thousand patients in a year, which is a much more compelling argument both for the public that this is safe and this can be the norm. It’s also a more compelling argument for my colleagues to show that this can be the norm—that people don’t have to wait.
Using that name as a descriptive was also important for selecting patients who would be good medical candidates—someone who would have a good interaction with that concept. For someone who wants a lot of counseling and a lot of soft touch, there are other providers who are offering that service via telehealth and I think it’d be a better fit for them. AOD is not set up to spend 30 minutes talking to a patient about whether they want to continue their pregnancy or not. It’s really meant for people who know they want an abortion and know they want a medication abortion and are comfortable with doing it at home themselves.
And then the other reason for the name Abortion on Demand is I’m sick of the euphemisms. I really am. I recognize that using the phrase “abortion on demand” is probably going to turn some patients off. But when I’m in 20 states, it’s okay if I lose some patients because of the word “abortion.” I think we should be calling it what it is. I don’t think the euphemisms are helpful. I recognize that’s an unusual lane to be in, in 2021 when there’s lots of pastel colors and animation and personalized services. AOD is as low-touch abortion as possible.
Baker: I hear you’re going to launch in seven more states. When will that happen?
Phifer: Definitely. Idaho will probably launch in August, Alaska and Hawaii by the end of 2021 and New Hampshire probably early 2022. Michigan and Pennsylvania are my pie-in-the-sky states. They’re purple states, so the state legislature is a risk regardless of what the law says and both of those states have some unusual laws that make it a little more challenging for us to provide care. It’s not impossible like it is in the ones where it says it’s restricted, but it’s pretty difficult at this point. And then Wyoming, gosh, Wyoming. It would be wonderful to provide care because it’s so rural. Telemedicine abortion is not outlawed in Wyoming by any means, but there’s some vague language about practicing outside of the norm. I have to kind of wait on Wyoming, but once I figure that out it will be ready to go.
Baker: Is there anything else you want folks to know?
Phifer: I think we’re making abortion more complicated than it needs to be. Abortion is not complicated. It’s not traumatic. The actual medicine behind it is really simple. It’s all of the other things that makes abortion complicated. Whatever we can do to remove that, the better.
Patients, a lot of them, don’t need a lot of counseling. A lot of people just know they want an abortion. I would love that the standard be less emphasis on what the provider thinks the patient wants and more emphasis on patient-driven care. AOD is essentially patient driven. They tell us what they want. We’re just making sure that the boundaries they give us are safe.
Up next:





