Examining nursing homes, prisons, jails, psychiatric hospitals and immigration detention centers through a disability lens allows for creative redesigns that question the very function of these institutions. It’s time to unite the movements for abolition, decarceration and defunding police, and invest in long-term, community-based solutions—rather than disconnected, piecemeal reforms.

This piece is part of “Women on the Frontlines: COVID and Beyond,” an online symposium examining the political, economic, social and legal status of women.
Sponsored by the Cornell Law Review with the Center for Biotechnology and Global Health Policy and co-hosted by Ms. and others, the symposium brings to light the ways women labor and lead at the forefront of society, constituting the foundation of essential workers, and performing critical services from child to medical care. But during the pandemic, women (especially women of color) suffer persistent economic constraints; health and death disparities; obstruction of rights; and the troubling perceptions of expendability. Watch “Women on the Frontlines: COVID and Beyond” for a discourse about the role of women and pathways toward a more just society.
The hotbeds of COVID-19 continue to be congregate “custodial spaces”—such as nursing homes, prisons, jails, psychiatric hospitals and immigration detention centers. By looking at the effects of COVID-19 in these spaces, we can also see an important dimension emerge: the effects on women of color on the frontlines and those with disabilities.

The current pandemic has raised the stakes—and, in some notable respects, cleared the way—for a modern deinstitutionalization movement, breaking down silos that have obscured the common experience of structural subordination across civil rights movements.
With the high percentage of people in custodial spaces who have disabilities, disability laws offer short-term, emergency interventions to move those with underlying health conditions out of these congregate settings.
Perhaps more importantly, examining nursing homes, prisons, jails, psychiatric hospitals and immigration detention centers through a disability lens allows for creative redesigns that question the very function of these institutions. It’s time to unite the movements for abolition, decarceration and defunding police, and invest in long-term, community-based solutions—rather than disconnected, piecemeal reforms.
Disparate Impacts of COVID-19
There are over 10.4 million infections and 240,000 deaths in the United States directly linked to COVID-19.
However, the effects are unevenly distributed: Black Americans account for 20 percent of COVID-19 deaths—a rate of death between two and three times that of white people. While Latinxs comprise 19 percent of the U.S. population, they represent over 21 percent of the COVID-19 death toll—over three times the death rate of whites. Indigenous Americans also have a death rate three times that of whites.
In prisons and jails, more than 252,000 people have been infected and at least 1,450 inmates and correctional officers have died of coronavirus. U.S. Immigration and Customs Enforcement (ICE) has reported only four COVID-related deaths of its detainees out of the 4,444 confirmed infections—a figure some advocates view with great skepticism because of how ICE collects and tracks COVID-19 data. (ICE only tracks COVID-19 deaths that take place within its custody, not cases of people infected while in detention who then die once released or deported.)

Similarly, although less than one percent of Americans live in long-term facilities, they account for 40 percent of U.S. COVID-19 deaths, as of Nov. 5.
Psychiatric hospitals providing inpatient care to people with psychiatric disabilities are also high-risk settings that manifest the dangers of custodial spaces. For example, by mid-April, New Jersey’s four psychiatric hospitals had over 200 infections and five deaths, with four of the five deaths at a single hospital. Approximately one in 10 people being treated at that hospital and 44 employees tested positive for COVID-19.
The Dangers of Custodial Spaces
Custodial spaces are those institutional settings such as prisons, jails, psychiatric hospitals, residential institutions for people with intellectual and developmental disabilities, ICE detention, nursing homes and long-term care facilities. They share three common elements that make them particularly susceptible to contagion:
- architectural designs,
- historic neglect, and
- perceptions of disposable populations.
First, architecture often reflects broader social visions of the institution being designed. For custodial spaces, that has historically been understood to mean a focus on containment, behavioral management and, at least in theory, safety. Custodial spaces are usually large-scale, remotely located complexes emphasizing surveillance and the absence of privacy.
The allocation of space to containment rather than social services—health, nutrition, education, enrichment—reflects the punitive nature of the setting even, as in the case of ICE detention, when the primary purpose is not retributive.
Pre-existing conditions in ICE facilities, for example, led two professional organizations to issue a statement calling for fellow architects to “condemn all policies that use the built environment as an instrument of torture and oppression” and “refuse to participate in the design of any immigration enforcement infrastructure, including but not limited to walls, checkpoints, [ICE] offices, detention facilities, processing centers, or juvenile holding centers.”
Consider nursing homes (even private ones) where “cluster neighborhood design” is the standard around the world—with up to 50 residents residing in a single wing (two to four people per room). Overcrowding, the absence of sufficient personal protective equipment (PPE) and cleaning supplies as well as the inability to social distance have placed employees and detainees at risk.
Second, custodial spaces are usually sites of historic neglect—the subject of impact cases that have produced relatively superficial compliance with structural reforms, making these institutions vulnerable to COVID-19.
Prisons and jails, for example, have endured countless lawsuits and subsequent consent decrees managed by federal court judges over decades. Rikers Island in New York City, for instance, was subject to several impact cases from the 1970s until about a decade ago for improper ventilation, extreme temperatures, poor sanitation, overcrowding, lack of adequate cleaning supplies and understaffing.
ICE detention facilities, even before the pandemic, were considered breeding grounds for contagion and lacking in medical care. For example, in Fraihat v. U.S. Immigrations and Customs Enforcement, a putative plaintiff class alleged systemic neglect in the provision of medical care and safe conditions for detainees that make detainees more susceptible now to COVID-19.
Third, custodial spaces provide residential care for politically or socially disfavored populations—people charged with or convicted of crimes, older adults, people with disabilities and undocumented individuals—leading to their treatment as more disposable especially during times of crisis.
For example, at the onset of the pandemic, medical professionals faced questions of how to allocate potentially scarce resources such as ventilators or hospital beds. Triage policies emerged (and were subsequently challenged by legal advocates)—that explicitly weighed the presence of certain disabilities (such as intellectual or developmental) and age as factors making some “poor candidates” for limited services.
We will likely see similar triage policies surface when a vaccine emerges.
COVID-19’s Ecosystems: Women and People with Disabilities
Although fewer women have died in prisons and jails relative to men in the same settings—leading to greater public invisibility in the media—the effects of COVID-19 on women present distinct challenges.
For example, approximately eighty percent of women in prisons are mothers, many who were single mothers before incarceration. Institutional policies such as restrictions or elimination of visiting policies leave women without connections to their families and children without connection to their mothers, resulting in greater mental health trauma and challenges all around. Pre-existing health conditions such as diabetes, heart disease, and asthma place women of color in congregate custodial spaces at greater risk for contracting and dying from COVID-19.
Framing the effects of COVID-19 on female-headed ecosystems allows us to better understand the extended networks of individuals and communities affected by the pandemic.
In addition, in certain industries, such as personal or health assistance in long-term facilities (often low-wage work), women of color are overrepresented: 82 percent of employees are female and 26 percent, a disproportionate share, are Black.
A Remedial Role for Law During the Pandemic?
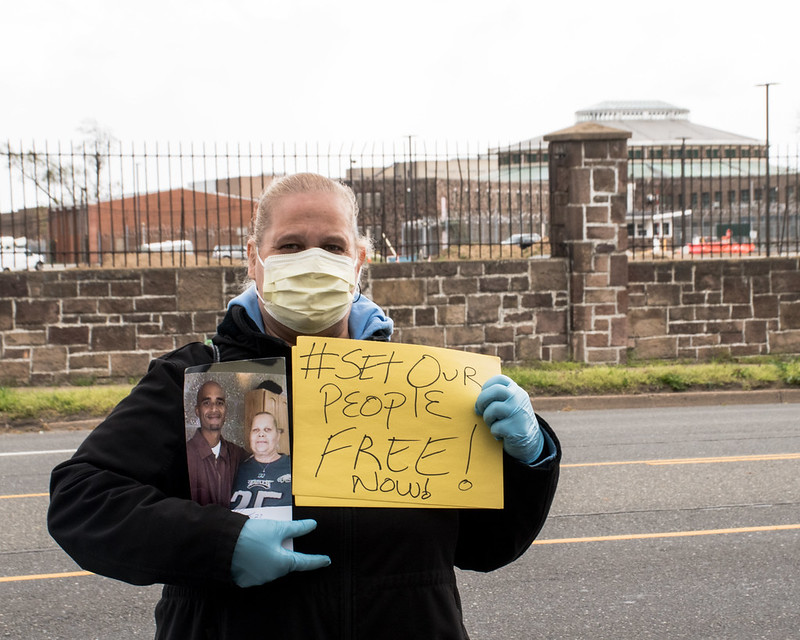
Most of the current litigation in custodial spaces tends to focus on the release of vulnerable populations housed in these institutions. Initially, prison cases, for example, focused on “compassionate release” of those non-violent individuals in prisons and those most medically vulnerable to COVID-19.
Other legal complaints have framed jail and prison confinement without the necessary public health compliance as “cruel and unusual” punishment in violation of the U.S. Constitution’s Eighth Amendment.
The critical challenge is time: As everyone tries to adapt to the new pandemic reality, courts appear to be reluctant to grant a mass release of people from jails and prisons, instead offering custodial spaces opportunities for reform or amelioration. Because federal courts, in particular, have been hostile to prison conditions cases (particularly after the Prison Litigation Reform Act), broadly framed decarceration efforts face an uphill battle.
Legal advocates may have greater success focusing on “vulnerable” populations in custodial spaces—particularly prisons and jails—using disability laws such as the Americans with Disabilities Act and Section 504 of the Rehabilitation Act of 1973 and framing release as a “reasonable modification” or through Olmstead enforcement actions. However, most litigation is in its nascent stage and will continue to develop.
While litigation may offer a short-term solution to transfer people in custodial spaces to relatively less risky community settings, the structural question remains: Can reform or redesign and abolition offer the better path forward?
Calls for prison abolition, decarceration, defunding the police, closing ICE facilities, psychiatric hospitals and nursing homes and investing in sustainable community based services and alternatives to punitive detention offer a different vision of care and interdependence that demands sufficient fiscal support from federal, state and local governments.
A common response to calls for broad institutional redesigns rather than reforms is that it would not be feasible or practical because, among other reasons proffered, it would be impossible to hit the stop button long enough to imagine and create alternative systems.
Although the dark cloud of COVID-19 feels all encompassing, the silver lining is that we have an opportunity to probe state institutions across a number of areas of law and collectively envision the responsibility of the state to the most vulnerable in our society.
You may also like:





