Now more than ever before, access to contraceptives must be expanded.
Unintended pregnancy—either unwanted or mistimed—is an important public health concern. Women who have unplanned pregnancies are more likely to delay prenatal care and suffer from postpartum depression. Although the unintended pregnancy rate in the U.S. is at an all-time low, recent data shows 45 percent of pregnancies are still unintended—higher than in many other industrialized nations. Adolescents (15-17 years of age), young adults (18-29 years of age), women with low income and educational attainment, and racial/ethnic minorities are disproportionately affected by unintended pregnancies. Most unintended pregnancies are due to non-use, inconsistent use or incorrect use of contraceptives. Several barriers, including cost and access, hinder women from getting contraceptives or using them consistently.
The COVID-19 pandemic and a recession have exacerbated these issues, with nearly 12 million women worldwide losing access to contraception due to pandemic disruptions. A survey found that one in three U.S. women experienced difficulties in accessing contraception since the start of the pandemic with Black, Hispanic and queer women being disproportionately impacted by these disruptions. Now more than ever before, access to contraceptives must be expanded.
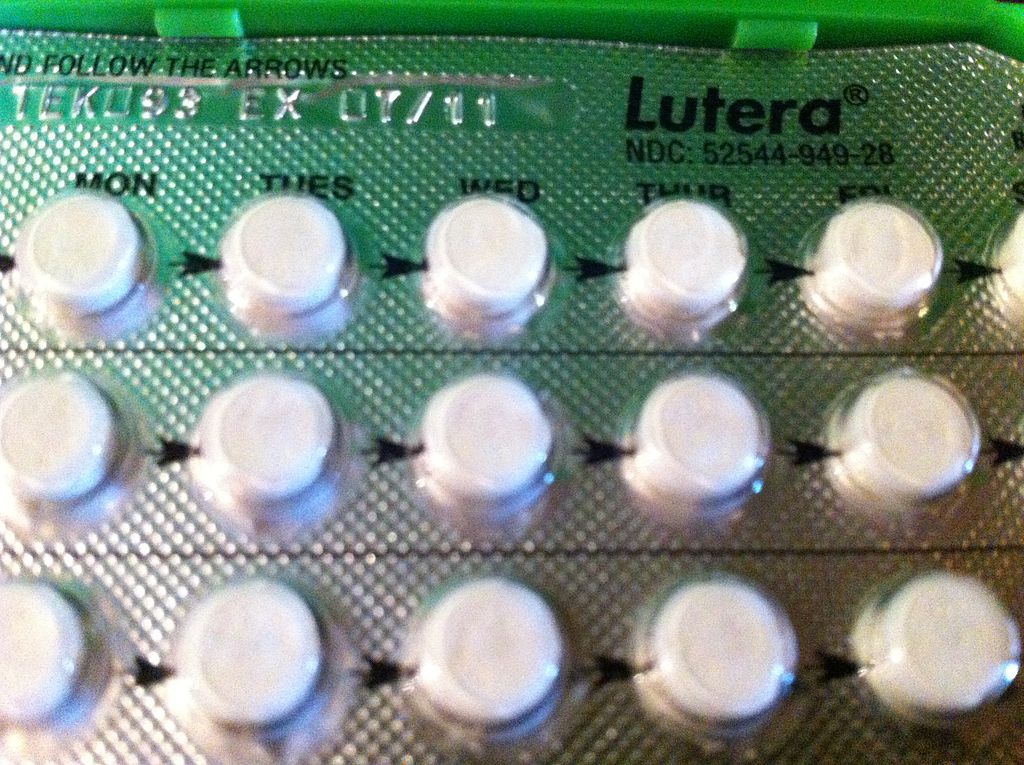
The second most used contraceptive method in the U.S., after female sterilization, is the oral contraceptive pill, or birth control pill. The U.S. is one of the few countries in the world that requires women to have a prescription to obtain birth control pills—which serves as a significant barrier, especially for those who lack access to a healthcare provider, transportation childcare and other resources. A national representative survey found 29 percent of women had difficulty getting a prescription or refill for birth control pills. Frequently reported barriers included cost- or insurance-related barriers, issues with scheduling an appointment or traveling to the doctor’s office, the doctor requiring a clinic visit, pelvic exam or Pap smear, and not having a primary care doctor. Making birth control pills available over the counter (OTC) will remove such barriers, increasing access to contraception for millions of women.
How to Switch from Prescription to Over-the-Counter (OTC) Access
To make a drug available OTC, drug manufacturers must submit a new drug application to the U.S. Food and Drug Administration (FDA). The FDA then assesses if the drug meets the following criteria:
- Acceptable safety margin with low misuse and abuse potential
- Adequate labeling that is understandable by the layperson
- No clinician is needed for the safe and effective use of the drug as consumers can self-diagnose the condition for which the drug is indicated for and self-screen for contraindications
Birth control pills have been approved for use for over 60 years now, so their side effect profile has been well-understood. They have a low misuse and abuse potential, as they are not addictive and do not cause severe toxicity if overdosed. Most side effects are benign like bleeding between periods and nausea. Serious complications are very rare.
The most frequently cited complication is the formation of blood clots due to the ethinyl estradiol—a form of estrogen—or certain progestin forms found in combined birth control pills. However, the absolute risk of blood clots among users of the combined birth control pill is still very low (7 out of 10,000 women), which is lower than the risk of blood clots during pregnancy (20 out of 10,000 women). Furthermore, the progestin-only birth control pill, sometimes called the minipill, is not associated with an increased risk for blood clots. Overall, the benefits outweigh the risks as birth control pills are safer than the alternatives of pregnancy and childbirth.
Like with many other OTC medications, birth control pills are not for everyone. Women with certain conditions should avoid combined birth control pills, while others should avoid progestin-only pills in order to minimize health risks—just like how some with asthma or peptic ulcer disease avoid using aspirin, an OTC drug. Research establishes that women are capable of self-screening for risk factors as effectively as their healthcare providers. One study found that women were able to accurately identify contraindications using a simple checklist.
What does all this mean? That birth control pills meet the FDA’s criteria to be made available without a prescription.
Women and Healthcare Providers Want Over-the-Counter (OTC) Birth Control Pills
A Kaiser survey showed three in four women supported making birth control pills available OTC. Another national survey found 62 percent of participants favored OTC birth control pills, and 37 percent would likely use birth control pills if they were made available OTC, including 28 percent of participants who were using no contraceptive method.
A study that aimed to understand which contraceptive features were valued by women found current prescription birth control pills only had 60 percent of the “extremely important features.” However, an OTC pill would have 71 percent of the valued features, making it a closer match with women’s preferences. Clinicians also support OTC birth control pills; both the American College of Obstetricians and Physicians and American Academy of Family Physicians support OTC access to birth control pills.
Ensuring Insurance Coverage and Access for All Ages
Under the Affordable Care Act’s contraceptive mandate, most private health insurance plans are required to cover the full range of contraceptive methods for women, without out-of-pocket costs to the patient. According to this mandate, insurance companies need to cover OTC contraceptives like female condoms and spermicides, but only if the woman has a prescription. So, if birth control pills become OTC, but the pills are expensive, then one barrier (access) will simply be replaced by another (cost). Coverage for OTC contraceptive methods needs to be strengthened by eliminating the prescription requirement for coverage of any OTC contraceptive method. The U.S. military’s Tricare insurance program covers OTC contraceptive products like Plan B without a prescription and could serve as a model for other insurance programs.
Provisions of the Affordability Is Access Act (AAA), which would ensure insurance coverage of FDA-approved OTC birth control pills without the need for a prescription, must be prioritized and enacted by policymakers.
Just like Plan B, birth control should be made available OTC with no age restrictions. Adolescents face higher rates of unintended pregnancies and more barriers to contraception access. They may fear their parents finding out if they schedule an appointment with their doctor to get a prescription or they may not have transportation to a doctor’s office—meaning adolescents have the most to gain from OTC access to birth control pills. Research further shows birth control pills are safe and effective in adolescents. In fact, potential contraindications to birth control pills are less frequent in adolescents compared to older women.
Teens are also interested in OTC birth control pills: A survey of adolescents aged 14-17 found that 73 percent of participants favored OTC access and 61 percent reported they would use OTC birth control pills.
OTC birth control pills, especially if covered by insurance, would be a game-changer for millions of women in America who experience barriers to contraception access. A study found that OTC birth control pills could reduce unintended pregnancies by as much as 25 percent.
As of now, two drug manufacturers, HRA Pharma and Cadence Health are seeking FDA approval for OTC birth control pills. Free the Pill, a campaign that supports affordable, insurance-covered OTC birth control pills, has been lobbying the FDA. Free the Pill originated out of the Oral Contraceptives (OCs) Over-the-Counter Working Group, a coalition of reproductive health and justice organizations, nonprofit research and advocacy groups, and clinicians who support greater access to safe and effective contraception.
To learn more about how you can also get involved in the movement for OTC birth control, visit https://freethepill.org/act/ or follow Free the Pill on social media.
U.S. democracy is at a dangerous inflection point—from the demise of abortion rights, to a lack of pay equity and parental leave, to skyrocketing maternal mortality, and attacks on trans health. Left unchecked, these crises will lead to wider gaps in political participation and representation. For 50 years, Ms. has been forging feminist journalism—reporting, rebelling and truth-telling from the front-lines, championing the Equal Rights Amendment, and centering the stories of those most impacted. With all that’s at stake for equality, we are redoubling our commitment for the next 50 years. In turn, we need your help, Support Ms. today with a donation—any amount that is meaningful to you. For as little as $5 each month, you’ll receive the print magazine along with our e-newsletters, action alerts, and invitations to Ms. Studios events and podcasts. We are grateful for your loyalty and ferocity.
Up next:





